Premium Medical Billing Solutions provides healthcare providers with comprehensive credentialing services. These services comprise verifying and assessing the provider’s qualifications and professional and training history. This ensures that the provider meets the standards required to practice in the USA.
This is a sensitive process that demands keen focus. In our medical credentialing services, we ensure quality care, maintain patient safety, and facilitate reimbursement from payor companies. Medical Credentialing is the basic step of medical billing. Without a a provider’s credentialing, the provider cannot work with payer companies. We know the importance of credentialing services and how to enroll a doctor in insurance companies.
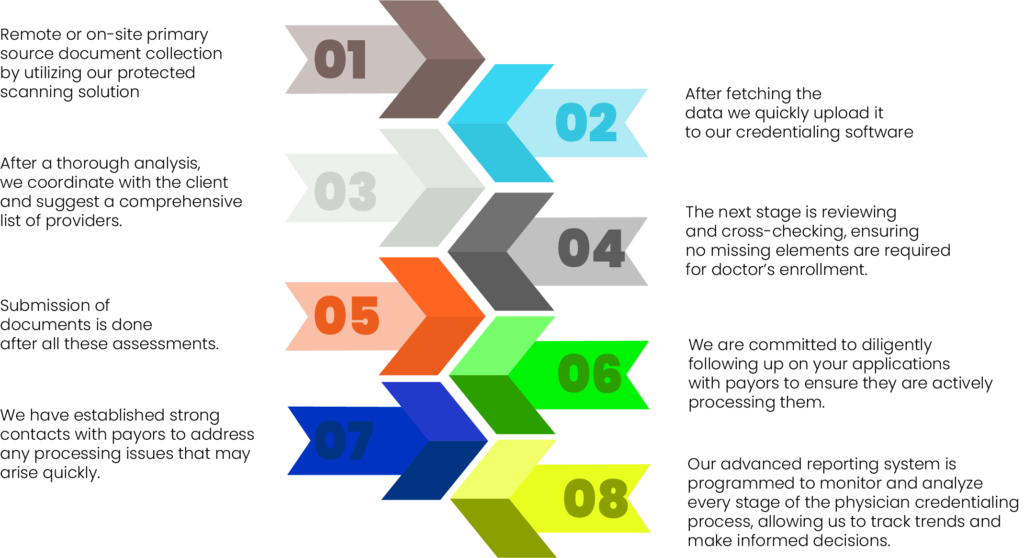
Our highly qualified experts do the job of credentialing in an optimum manner and within the specified time frame. Here are some essential requirements needed for credentialing and see how our expert does this job professionally by collecting:
There are certain benefits we provide to our clients in terms of providing credentialing medical services. These benefits are lucrative in providing easy enrollment of the practitioner in the insurance company but also play a vital role in boosting RCM. A boosted RCM equals high revenue.

Understanding that the credentialing process doesn’t end once a provider gets into a payer’s network is important. Providers must undergo routine screening and license verification to ensure compliance and quality care toward patients. This ongoing process, known as re-credentialing, involves periodic screening and verification. Re-credentialing is essential to confirm a provider’s training and qualifications and detect fraud or abuse. While credentialing can be complex and time-consuming, neglecting it can have severe consequences.
Conduct all re-credentialing services based on insurance plans and requirements.
Advance management and consolidation of application and signature page
Use of fastest mailing services to perform the re-credentialing process without any adu
Punctual and efficient application follow-ups are made to confirm if the payor company is processing the application
With years of experience and a dedicated team of credentialing experts, we specialize in handling all aspects of the credentialing process, including initial credentialing, re-credentialing, and provider enrollment for both in-network and out-of-network providers. We aim to ensure you are credentialed and contracted with all major payers, allowing you to focus on what you do best – providing exceptional patient care.
Our provider enrollment and credentialing services help you avoid delays in claim submission and confusion with insurance enrollment. Whether you are looking for Medicare provider enrollment or Medicaid provider enrollment, we have the answer to every question. Our medical credentialing specialist lets you start with documentation and sign up for commercial and non-commercial insurance. We share a complete insight into submitted applications, help create insurance portals, and ensure compliance with NCQA and DHFS.
Getting started is easy! Simply contact us to schedule a consultation, and we'll guide you through the process and tailor our services to meet your unique needs and requirements.
Yes, we offer ongoing support to assist with any updates, changes, or inquiries regarding your credential status and re-credentialing when necessary to maintain your participation in insurance networks.
Of course, we offer enrollment assistance in Medicare, Medicaid, and other government healthcare programs to ensure you are properly registered and eligible to provide services to patients.
Yes, we provide comprehensive services for initial credentialing upon joining a new network or plan and re-credentialing to maintain your participation status and ensure ongoing compliance.
Basic requirements for provider credentials typically include proof of licensure, relevant education, training, board certification, malpractice insurance, and work history.
30 N Gould St, Sheridan, WY 82801, USA
Copyright © 2024 Premium Medical Billing Solutions LLC. All rights reserved.